Author Affiliations
Abstract
Chronic obstructive pulmonary disease (COPD), heart failure (HF), interstitial lung disease (ILD), and hypertension (HTN) are major contributors to global morbidity, disability, and healthcare burden. These conditions are associated with persistent symptoms, impaired quality of life, high hospitalization rates, and increased mortality. Despite guideline recommendations, access to integrated palliative care and rehabilitation remains limited, while conventional disease management often overlooks psychosocial and functional needs. Advances in telemedicine and mobile health (mHealth) offer potential to bridge these gaps.
The advancing symptom alleviation with palliative treatment (ADAPT) randomized clinical trial evaluated a nurse-social worker telecare team in Veterans Health Administration systems, showing significant improvements in quality of life, depression, and anxiety among patients with COPD, HF, or ILD, though hospitalization and mortality were unaffected. A Norwegian trial of telerehabilitation in patients with chronic heart failure (CHF) demonstrated high adherence, safety, and satisfaction with remote high-intensity interval training, as well as improved functional outcomes compared to declines in controls. In Singapore, qualitative interviews revealed that blood pressure (BP) telemonitoring enhanced convenience, discipline, and self-management, though usability challenges and technology anxiety persisted. In China, the intelligent hypertension excellence centers (iHEC) randomized trial reported greater reductions in systolic blood pressure (SBP), improved control rates, and fewer excessive reductions among older adults, with strong engagement in remote consultations and monitoring.
These findings emphasize the effectiveness and feasibility of patient-centered, technology-enabled care models. While mortality outcomes remain unchanged, improvements in quality of life, functional capacity, and blood pressure control highlight the potential of scalable interventions to transform chronic disease management.
Keywords
Telerehabilitation, Chronic obstructive pulmonary disease, Heart failure, Interstitial lung disease, Blood pressure telemonitoring.
Introduction
COPD, HF, and ILD cause high morbidity and poor quality of life due to persistent symptoms like breathlessness, fatigue, pain, and sleep disturbance. Depression and anxiety are also common, with significant overlap between HF and COPD. Despite international guidelines recommending palliative care integration, access to outpatient palliative care in the U.S. remains limited, and current disease management programs focus mainly on disease-specific therapies. Given workforce shortages, new scalable care models are needed.[1-7]
CHF affects about 26 million people worldwide, with prevalence rising due to aging populations and improved treatments. CHF carries high mortality, frequent hospitalizations, reduced quality of life, and substantial economic costs. A key feature is impaired blood flow, often evident during exercise. Exercise-based cardiac rehabilitation (CR) improves capacity, quality of life, and reduces hospitalizations, earning a Class I recommendation. High-intensity interval training is a safe and effective exercise regimen for patients with CHF. However, many patients remain inactive due to barriers like age, frailty, cost, and distance. Novel strategies, including telerehabilitation, may enhance access to and adherence with CR programs.[8-15]
HTN affects 35.5% of adults in Singapore and is a major primary care concern locally and worldwide. Globally, elevated blood pressure ranks among the top five causes of attributable deaths and is a key risk factor for ischemic heart disease and stroke, leading contributors to disability-adjusted life years in older adults. Management includes lifestyle modification and pharmacological therapy, but telemedicine is increasingly integrated to enhance access, care quality, and prevention of cardiovascular disease.[16-21] In Singapore, telemedicine encompasses tele-collaboration, tele-treatment, tele-monitoring, and tele-support, with BP telemonitoring emerging as the most effective and widely adopted tool for HTN management.[22,23]
HTN is the leading risk factor for cardiovascular disease, affecting 350 million people in China, over half of whom are older adults. Yet, only about 15% achieve blood pressure control. Older patients face unique barriers, including cognitive decline, mobility issues, registration difficulties, and high medical costs, leading to poor compliance and follow-up. SBP is most critical in predicting organ damage and cardiovascular events, but excessive SBP reduction increases risks of dizziness, falls, and fractures, especially in frail patients. With the growing use of smartphones, mobile health apps present new opportunities, although their effectiveness in older populations remains uncertain.[24-26]
Methodology
A systematic literature search was conducted to identify recent clinical evidence on the role of telemedicine in the management of chronic diseases, particularly chronic obstructive pulmonary disease (COPD), heart failure (HF), interstitial lung disease (ILD), and hypertension (HTN). The PubMed database was searched for articles published between January 2023 and January 2025, ensuring that only the most up-to-date studies were included.
The following keywords and combinations were used: “Telemedicine” OR “Telehealth” OR “Remote consultation” OR “eHealth” AND “Chronic disease” OR “Interstitial lung disease” OR “COPD” OR “Heart failure”. Filters were applied to restrict results to clinical trials and randomized controlled trials (RCTs). Only publications in English were considered.
Inclusion criteria
- Clinical trials and randomized controlled trials
- Studies involving human subjects
- Articles published in English within the defined time frame
Exclusion criteria
- Books, commentaries, editorials, letters, and book chapters
- Case reports, case series, and literature reviews
- Animal or in vitro (laboratory) studies
- Studies lacking a reported results section
Titles and abstracts were screened for relevance, and full texts of eligible studies were reviewed. The included studies were narratively synthesized to highlight the role of telemedicine in improving quality of life, functional outcomes, self-management, and blood pressure control in patients with chronic cardiopulmonary and cardiovascular diseases.
A total of 1,388 records were initially identified through database searches. Before screening, 1,032 records were removed for various reasons, including duplication, irrelevance, or failure to meet the inclusion criteria. The remaining 356 records were screened, of which 149 were excluded after reviewing the title and abstract. From the remaining 207 records, 153 could not be retrieved in full text. A total of 54 full-text reports were then assessed for eligibility. Among these, 50 studies were excluded due to a low SANRA quality score (<10). Finally, four studies met the inclusion criteria and were included in this review.
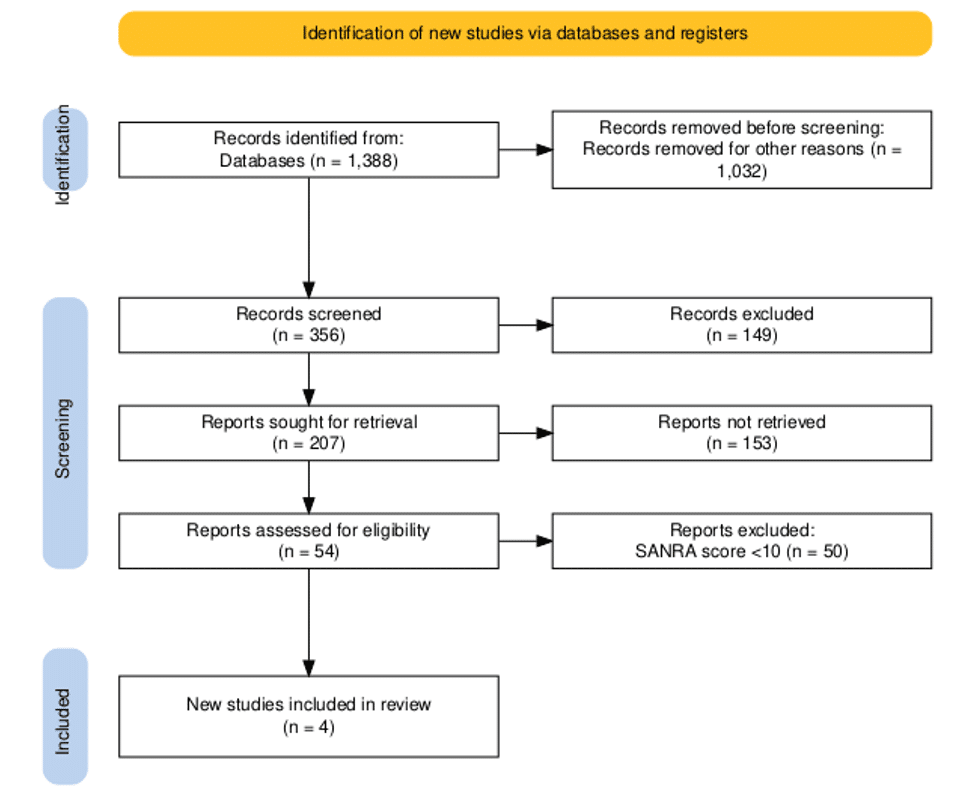
Figure 1: PRISMA flow diagram
Results
Participant characteristics, intervention delivery, and clinical outcomes: Bekelman DB et al. The ADAPT study was a single-blind, two-group randomized clinical trial comparing a nurse–social worker palliative telecare team with usual care in two Veterans Health Administration systems (Colorado and Washington). Eligible patients were identified through electronic health records using the following criteria: COPD, HF, or at least two outpatient visits; ILD was added in May 2018. Patients in the top 20th percentile of risk for hospitalization or death within 1 year (with a probability of 16%-98%) were screened. Exclusions included metastatic cancer, substance misuse, incarceration, pregnancy, or prior Collaborative Care to Alleviate Symptoms and Adjust to Illness (CASA) participation. Additional criteria were poor quality of life, Functional Assessment of Chronic Illness Therapy–General (FACT-G ≤70), bothersome symptoms, primary care access, not living in a nursing home, reliable phone access, and no prior lung/heart transplant. Consenting patients completed baseline measures and were randomized using concealed, computer-generated blocks stratified by site and disease. Recruitment occurred from October 2016 to April 2020.
The ADAPT intervention applied a collaborative care model. A nurse addressed symptoms, and a social worker provided structured counseling, each aiming for six phone sessions (twice monthly) tailored to the patient’s needs. Initial nurse calls targeted one symptom (pain, fatigue, depression, dyspnea, or sleep disturbance) using structured guidelines and motivational interviewing. Social workers delivered psychosocial counselling on coping, adjustment, and care goals. Weekly, the intervention team reviewed cases with clinicians, palliative specialists, and subspecialists. The primary outcome was the change in quality of life at 6 months (FACT-G). Secondary outcomes included disease-specific quality of life, mood, hospitalizations, and mortality. A sample size of 300 (with 85% power and α = 0.05) was planned, allowing for 25% attrition. Analyses used linear and generalized linear mixed models with maximum likelihood estimation, stratified by disease and time.
A total of 8492 patients with COPD, HF, or ILD codes were screened; 5759 were excluded due to disease severity or quality-of-life criteria. Recruitment goals were achieved, with 306 participants randomized (154 ADAPT intervention, 152 usual care). The cohort was predominantly male (90.2%) and White (80.1%), with a mean age of 68.9 (7.7) years. Education and income varied, with 28% completing high school or less and 58% reporting annual income ≤$40,000. Diagnoses included COPD (58%), HF (22%), COPD with HF (16%), and ILD (4%). Nearly half had been hospitalized within the past year, and 21% had had two or more admissions. Mental health care was common, with 28% on medication and 32% receiving counselling. Among intervention patients, 112 (73%) received the program, averaging 10.4 calls over a period of 115 days. Fidelity exceeded 98%. At 6 months, FACT-G scores improved more with the intervention (mean difference, 4.6; P = .001), with benefits observed across COPD, HF, depression, and anxiety, which persisted at 4 and 12 months. No intervention harms occurred; hospitalization and 1-year mortality rates were similar.[27]
Baseline characteristics, adherence, safety, and functional outcomes: This prospective randomized controlled trial by Lundgren KM allocated CHF patients 1:1 to telerehabilitation or control for 3 months, stratified by age (<60/≥60 years) and LVEF (<40/≥40%). Randomization was conducted centrally at NTNU, Trondheim. Outcomes were measured at baseline, at the end of the intervention (24 exercise sessions or 3 months), and at the 3-month follow-up. The study was approved by the Regional Ethics Committee (2016/1597), with written informed consent obtained. A total of 61 patients (≥18 years old) with reduced (≤40%), mildly reduced (41-49%), or preserved (≥50%) were recruited in Norway (2017-2020). Inclusion required stable therapy >4 weeks; exclusions were recent CR (<6 months), reversible CHF, severe pulmonary disease (COPD GOLD III–IV), or unsafe home exercise. All participants underwent baseline examinations, including echocardiography, as well as a 2-day “Living with Heart Failure” course. The telerehabilitation group completed 24 high-intensity interval sessions (85-95% HRmax) via videoconferencing, twice weekly for 60 minutes, with safety monitoring and supplementary resources.
The primary outcome was feasibility (adherence, safety, satisfaction, technical issues). Secondary outcomes were self-efficacy, physical fitness, and functional performance. Analyses used linear and logistic mixed models (intention-to-treat), with per-protocol defined as ≥80% adherence. Between June 2017 and April 2019, 231 patients with CHF were assessed, and 61 were randomized (31 to telerehabilitation and 30 to control). Baseline characteristics were comparable across groups, with minor, non-significant differences in body mass index (BMI) and N-terminal pro-brain natriuretic peptide (NT-proBNP). Participants were predominantly male (82%), with a mean age of 67.6 years. Most were married (57.4%), had a high school education (45.9%), and were independent in activities of daily living (86.9%). The majority were New York Heart Association (NYHA) class II (82%). Comorbidities included HTN (54.1%), diabetes (27.9%), and atrial fibrillation/flutter (45.9%). Common medications included β-blockers (91.8%), ACE inhibitors/ARB (90.2%), and diuretics (78.7%).
Adherence was high in the telerehabilitation group: 80.6% were adherent or partly adherent, with a median of 25 inter‐quartile range (IQR 21-28) sessions completed over 5 months (IQR 4.5-7.0). Heart rate monitoring in eight participants showed exercise intensities between 80% and 95% of HR peak across intervals. No session-related adverse events occurred; one hypoglycemia incident followed an unsupervised session. Two participants accounted for 41% of 22 AEs/SAEs in the telerehabilitation arm, and two accounted for 69% of 13 AEs/SAEs in controls.
Patient feedback showed 96% felt safe and motivated to continue exercising; however, 59% reported technical challenges. No significant between-group differences were observed for self-efficacy. In functional outcomes, peak oxygen uptake (VO₂peak) declined significantly in the control group (-0.72 mL/kg/min; P=0.03) but remained stable in the intervention group. The 6-minute walk test (6MWT) increased by 19.1 m (P=0.02) in the telerehabilitation group and 15.3 m (P=0.07) in controls, without significant between-group differences. Short Physical Performance Battery (SPPB) scores showed no group differences.[28]
Participant characteristics, usability challenges, and user experiences: In Teo SH. To capture diverse experiences of the intervention, the research team purposively recruited 20 patients who remained in the trial and 10 health care professionals (HCPs) involved in implementation. Patients were invited via telephone to achieve variation in age and sex, while HCPs were invited by email. Due to ethical approval limits, patients who withdrew could not be included. Semi-structured interviews were used to explore perceptions of the BP telemonitoring intervention. The topic guide, informed by study aims, literature, and team discussions, was pilot-tested and covered experiences with telemonitoring equipment, BP self-monitoring, teleconsultation, medication adjustments, and lifestyle changes. It was iteratively refined as data collection and analysis proceeded. All participants provided written consent. Interviews were conducted face-to-face between March and September 2019 in English or Mandarin by two trained investigators in private polyclinic rooms. Each lasted 20–60 minutes, was audio-recorded, transcribed verbatim, and anonymized. Repeat interviews were not conducted. Ethical approval was granted by the National Healthcare Group Domain Specific Review Board.
Data were analysed using the framework method. Transcripts were verified, repeatedly read, and independently coded by two researchers. Analyses were inductive, with patient and HCP data assessed separately. A reflexivity journal was maintained, and coding differences were resolved by consensus. Data were charted into a matrix to develop themes, which were then mapped to the socio-technical systems (STS) model. Saturation was reached after 21 interviews. Thirteen patients and eight HCPs participated. Patients were mostly male (61.5%), with a mean age of 55.7 years, and predominantly Chinese (92.3%); 69.2% had pre-university/tertiary education and full-time employment. HCPs were mainly female (87.5%), all Chinese, including family physicians, nurse clinicians, care managers, and coordinators with 1.5-40 years of practice.
Patients generally found devices easy to use but faced issues with ill-fitting cuffs (n=4) and connectivity problems. Many, especially educated patients and HCPs, suggested more user-friendly, integrated systems. Some patients desired access to BP records for trend monitoring, while HCPs raised concerns over confidentiality and portal inefficiency. Older patients reported technology anxiety, whereas working individuals valued convenience. Teleconsultations were appreciated, but occasionally interfered with work schedules. Younger, educated, and tech-adaptable participants were more receptive to remote care, while older patients preferred in-person consultations.[29]
Participant characteristics, BP outcomes, and intervention effects: Jiang Y et al. conducted a prospective, non-blinded randomized controlled trial between January-June 2022, with follow-up until June 30, 2023. The study was approved by the Institutional Review Committee of Sichuan Provincial People’s Hospital (No. 230, 2022) and complied with the Declaration of Helsinki; informed consent was obtained. Participants aged 60-80 years with hypertension, as defined by the 2019 Chinese guideline, were recruited from community medical centers. Inclusion required smartphone use and community residency; exclusions were major cardiovascular events, severe comorbidities, or refractory hypertension. General practitioners screened participants, who were randomized 1:1 via SAS 9.4 to intervention (conventional therapy + iHEC) or control (conventional therapy). Randomization balanced age, sex, baseline BP, smoking, and drinking. Both groups received calibrated Omron BP73A3T monitors and training. Baseline data included demographics, social history, BP, medications, frailty (FRAIL score), and cognition (Mini-Cog).
The intervention also used iHEC, comprising a patient-facing app for BP monitoring, reminders, and consultations; a web platform for remote management; and an educational official account. The primary outcome was SBP after 12 months, adjusted for baseline SBP and sex. Secondary outcomes included BP control, excessive BP reduction, and iHEC use. Based on sample size calculations, 540 patients were enrolled. Analyses followed intention-to-treat principles with linear regression (SAS 9.3), significance at P<0.05. From eight community medical service centers in six Chinese provinces/municipalities, 1074 participants were screened, and 540 were randomized equally into intervention (n=270) and control (n=270) groups. During follow-up, all uploaded BP data; 519 completed the trial (261 intervention, 258 control). After excluding two with missing data, 517 (95.7%) were analysed. The mean age was 71.4 ± 3.7 years; 38.3% were women. Most were Han (intervention 86.2%, control 88.7%). Baseline characteristics, including education, frailty, BMI, lifestyle, and comorbidities, were comparable.
Median baseline SBP was 149 mmHg in the intervention group and 148 mmHg in controls. At 12 months, SBP reductions were greater in the intervention group (-12 vs. -8 mmHg), with an adjusted between-group difference of -4.2 mmHg (95% confidence interval (CI): -6.4 to -2.0; P<0.001). DBP decreased similarly between groups (7 vs- -6 mmHg; adjusted difference -1.4 mmHg; P>0.05). Subgroup analyses showed no heterogeneity. BP control improved more in the intervention group (36.4% vs. 22.3%, P<0.05), especially in those on baseline therapy (33.5% vs. 14.1%, P<0.01). Excessive BP reduction was less frequent (3.8% vs. 9.0%, P<0.05), particularly among frail patients (2.5% vs. 19.5%). Intervention patients logged 23,752 home BP readings, 24,445 online consultations, and 361 remote therapy adjustments, with higher use among older, frail, and educated participants.[30]
| Study | Population | Intervention | Primary outcomes | Secondary outcomes |
| Bekelman DB et al. (JAMA, 2024) |
306 patients (COPD, HF, ILD); mean age 68.9 yrs; 90% male | Nurse–social worker telecare team (symptom mgmt + counselling, phone-based) | QoL improvement (FACT-G, +6 vs +1.4; p=0.001); reduced depression/anxiety | No differences in hospitalizations or mortality (3.9% vs 3.3%) |
| Lundgren KM et al. (ESC Heart Fail, 2023) |
61 CHF patients; mean age 67.6 yrs; 82% male | Telerehabilitation: remote high-intensity interval training via video (24 sessions) | Feasibility, adherence (80.6%); safety confirmed | VO₂ peak stable in intervention, declined in controls; 6MWT improved in intervention (+19m) |
| Teo SH et al. BMC Prim Care, 2023) |
13 patients + 8 HCPs; mean age 55.7 yrs; 61.5% male | BP telemonitoring with teleconsultations, socio-technical evaluation | Usability, patient/HCP experiences (convenience vs technical challenges) | Improved self-management, but tech anxiety in older patients |
| Jiang Y et al. (Hypertens Res, 2025) |
540 hypertensive patients; age 60–80 yrs; mean 71.4 yrs | iHEC model: smartphone app, web platform, online consultations, education | SBP reduction greater in intervention (−12 vs −8 mmHg; adj diff −4.2 mmHg, p<0.001) | Improved BP control rates (36.4% vs 22.3%); fewer excessive reductions (3.8% vs 9.0%) |
Table 1: Summary of studies
Discussion
While several recent studies (2023–2025) report improvements in quality of life, functional outcomes, and blood pressure control, evidence for reduced hospitalization or mortality remains limited. Across chronic cardiopulmonary and cardiovascular diseases, these trials collectively demonstrate the value of patient-centered, technology-assisted interventions. In the ADAPT study, integrating a nurse–social worker palliative telecare team significantly improved quality of life, depression, and anxiety in patients with COPD, HF, or ILD. Although hospitalization and mortality did not differ from usual care, sustained benefits highlight the feasibility of collaborative palliative models that extend support beyond traditional specialty services. Similarly, the telerehabilitation trial for CHF patients demonstrated high adherence, safety, and satisfaction with remotely supervised high-intensity interval training. Compared with controls, telerehabilitation stabilized VO₂peak and improved 6MWT performance, indicating its capacity to maintain functional outcomes while addressing barriers and costs that often limit participation.
Digital health also shows promise in HTN management. In Singapore, qualitative findings revealed that BP telemonitoring enhanced convenience, self-management, and engagement, though usability challenges and technology anxiety, especially among older patients, remained obstacles. The iHEC trial in China quantitatively confirmed the clinical potential, with greater reductions in SBP, higher control rates, and fewer excessive BP reductions, particularly in frail patients. Strong patient engagement with home monitoring and remote consultations demonstrated feasibility within community primary care. These trials emphasize a shift from disease-specific programs toward integrated, scalable care models. While hard outcomes like mortality may remain unchanged, improvements in quality of life, adherence, functional capacity, and blood pressure control are clinically meaningful.
Conclusion
These studies collectively highlight the growing importance of integrating palliative care, rehabilitation, and digital health technologies into the management of chronic cardiopulmonary and cardiovascular diseases. The ADAPT trial demonstrated that a nurse–social worker telecare team can meaningfully improve quality of life, depression, and anxiety in patients with COPD, HF, or ILD, even without significant changes in hospitalization or mortality. Similarly, the telerehabilitation study showed that remotely supervised high-intensity interval training is feasible, safe, and well accepted by CHF patients, stabilizing VO₂ peak and improving functional outcomes in comparison with declines observed in controls.
In HTN management, both qualitative and quantitative findings underscore the utility of telemedicine. Patients and providers in Singapore valued BP telemonitoring for its convenience and support in self-management, despite challenges with usability and technology anxiety. In China, the iHEC trial confirmed significant improvements in SBP reduction, control rates, and safety, particularly in frail older adults, with high engagement in home monitoring and online consultations.
Together, these findings reflect a paradigm shift from traditional, disease-specific programs toward scalable, patient-centered models that leverage technology to enhance access, adherence, and outcomes. Future work should focus on addressing digital literacy gaps, optimizing usability, and evaluating long-term cost-effectiveness to support broad implementation.
References
- Rezende LC, Ribeiro EG, Parreiras LC, et al. Telehealth and telemedicine in the management of adult patients after hospitalization for COPD exacerbation: a scoping review. J Bras Pneumol. 2023;49(3):e20220067. doi:10.36416/1806-3756/e20220067
PubMed | Crossref | Google Scholar - Romaszko-Wojtowicz A, Jaśkiewicz Ł, Jurczak P, Doboszyńska A. Telemedicine in Primary Practice in the Age of the COVID-19 Pandemic-Review. Medicina (Kaunas). 2023;59(9):1541. doi:10.3390/medicina59091541
PubMed | Crossref | Google Scholar - Ladds E, Khan M, Moore L, Kalin A, Greenhalgh T. The impact of remote care approaches on continuity in primary care: a mixed-studies systematic review. Br J Gen Pract. 2023;73(730):e374-e383. doi:10.3399/BJGP.2022.0398
PubMed | Crossref | Google Scholar - Gordon M, Sinopoulou V, Lakunina S, Gjuladin-Hellon T, Bracewell K, Akobeng AK. Remote care through telehealth for people with inflammatory bowel disease. Cochrane Database Syst Rev. 2023;5(5):CD014821. doi:10.1002/14651858.CD014821.pub2
PubMed | Crossref | Google Scholar - Rajkumar E, Gopi A, Joshi A, et al. Applications, benefits and challenges of telehealth in India during COVID-19 pandemic and beyond: a systematic review. BMC Health Serv Res. 2023;23(1):7. doi:10.1186/s12913-022-08970-8
PubMed | Crossref | Google Scholar - Rettinger L, Kuhn S. Barriers to Video Call-Based Telehealth in Allied Health Professions and Nursing: Scoping Review and Mapping Process. J Med Internet Res. 2023;25:e46715. doi:10.2196/46715
PubMed | Crossref | Google Scholar - Chakraborty I, Edirippulige S, Vigneswara Ilavarasan P. The role of telehealth startups in healthcare service delivery: A systematic review. Int J Med Inform. 2023;174:105048. doi:10.1016/j.ijmedinf.2023.105048
PubMed | Crossref | Google Scholar - Pegoraro N, Rossini B, Giganti M, et al. Telemedicine in Sports under Extreme Conditions: Data Transmission, Remote Medical Consultations, and Diagnostic Imaging. Int J Environ Res Public Health. 2023;20(14):6371. doi:10.3390/ijerph20146371
PubMed | Crossref | Google Scholar - Aung H, Tan R, Flynn C, et al. Digital remote maintenance inhaler adherence interventions in COPD: a systematic review and meta-analysis. Eur Respir Rev. 2024;33(174):240136. doi:10.1183/16000617.0136-2024
PubMed | Crossref | Google Scholar - Mehraeen E, SeyedAlinaghi S, Heydari M, et al. Telemedicine technologies and applications in the era of COVID-19 pandemic: A systematic review. Health Informatics J. 2023;29(2):14604582231167431. doi:10.1177/14604582231167431
PubMed | Crossref | Google Scholar - Pickard Strange M, Booth A, Akiki M, Wieringa S, Shaw SE. The Role of Virtual Consulting in Developing Environmentally Sustainable Health Care: Systematic Literature Review. J Med Internet Res. 2023;25:e44823. doi:10.2196/44823
PubMed | Crossref | Google Scholar - Shibata S, Hoshide S. Current situation of telemedicine research for cardiovascular risk in Japan. Hypertens Res. 2023;46(5):1171-1180. doi:10.1038/s41440-023-01224-y
PubMed | Crossref | Google Scholar - Dhunnoo P, Kemp B, McGuigan K, Meskó B, O’Rourke V, McCann M. Evaluation of Telemedicine Consultations Using Health Outcomes and User Attitudes and Experiences: Scoping Review. J Med Internet Res. 2024;26:e53266. doi:10.2196/53266
PubMed | Crossref | Google Scholar - Seng JJB, Gwee MFR, Yong MHA, Kwan YH, Thumboo J, Low LL. Role of Caregivers in Remote Management of Patients With Type 2 Diabetes Mellitus: Systematic Review of Literature. J Med Internet Res. 2023;25:e46988. doi:10.2196/46988
PubMed | Crossref | Google Scholar - Sousa VLP, Dourado Júnior FW, Anjos SJSBD, Moreira ACA. Nursing teleconsultation in primary health care: scoping review. Rev Lat Am Enfermagem. 2024;32:e4329. doi:10.1590/1518-8345.7212.4329
PubMed | Crossref | Google Scholar - Bowman M, Jalink M, Sharpe I, Srivastava S, Wijeratne DT. Videoconferencing interventions and COPD patient outcomes: A systematic review. J Telemed Telecare. 2024;30(7):1077-1096. doi:10.1177/1357633X231158140
PubMed | Crossref | Google Scholar - Anil K, Bird AR, Bridgman K, et al. Telehealth competencies for allied health professionals: A scoping review. J Telemed Telecare. 2025;31(4):487-499. doi:10.1177/1357633X231201877
PubMed | Crossref | Google Scholar - Ten Haaft BHEA, Montorsi RM, Barsom E, Kazemier G, Schijven MP, Besselink MG. Online video versus face-to-face patient-surgeon consultation: a systematic review. Surg Endosc. 2024;38(12):7064-7072. doi:10.1007/s00464-024-11307-7
PubMed | Crossref | Google Scholar - Campbell K, Greenfield G, Li E, et al. The Impact of Virtual Consultations on the Quality of Primary Care: Systematic Review. J Med Internet Res. 2023;25:e48920. doi:10.2196/48920
PubMed | Crossref | Google Scholar - Esposito S, Sambati V, Fogliazza F, Street ME, Principi N. The impact of telemedicine on pediatric type 1 diabetes management: benefits, challenges, and future directions. Front Endocrinol (Lausanne). 2024;15:1513166. doi:10.3389/fendo.2024.1513166
PubMed | Crossref | Google Scholar - Peeters KMM, Reichel LAM, Muris DMJ, Cals JWL. Family Physician-to-Hospital Specialist Electronic Consultation and Access to Hospital Care: A Systematic Review. JAMA Netw Open. 2024;7(1):e2351623. doi:10.1001/jamanetworkopen.2023.51623
PubMed | Crossref | Google Scholar - Zhang J, Ji X, Xie J, Lin K, Yao M, Chi C. Effectiveness of synchronous teleconsultation for patients with type 2 diabetes mellitus: a systematic review and meta-analysis. BMJ Open Diabetes Res Care. 2023;11(1):e003180. doi:10.1136/bmjdrc-2022-003180
PubMed | Crossref | Google Scholar - Tong SYK, Jackson TM, Lau AYS. Virtual physical examination in teleconsultation: A scoping review. Int J Med Inform. 2024;191:105561. doi:10.1016/j.ijmedinf.2024.105561
PubMed | Crossref | Google Scholar - Ford J, Reuber M. Comparisons of Communication in Medical Face-To-Face and Teleconsultations: A Systematic Review and Narrative Synthesis. Health Commun. 2024;39(5):1012-1026. doi:10.1080/10410236.2023.2201733
PubMed | Crossref | Google Scholar - Cunha AS, Pedro AR, Cordeiro JV. Facilitators of and Barriers to Accessing Hospital Medical Specialty Telemedicine Consultations During the COVID-19 Pandemic: Systematic Review. J Med Internet Res. 2023;25:e44188. doi:10.2196/44188
PubMed | Crossref | Google Scholar - Dinh A, Yin AL, Estrin D, Greenwald P, Fortenko A. Augmented Reality in Real-time Telemedicine and Telementoring: Scoping Review. JMIR Mhealth Uhealth. 2023;11:e45464. doi:10.2196/45464
PubMed | Crossref | Google Scholar - Bekelman DB, Feser W, Morgan B, et al. Nurse and Social Worker Palliative Telecare Team and Quality of Life in Patients With COPD, Heart Failure, or Interstitial Lung Disease: The ADAPT Randomized Clinical Trial. JAMA. 2024;331(3):212-223. doi:10.1001/jama.2023.24035
PubMed | Crossref | Google Scholar - Lundgren KM, Langlo KAR, Salvesen, et al. Feasibility of telerehabilitation for heart failure patients inaccessible for outpatient rehabilitation. ESC Heart Fail. 2023;10(4):2406-2417. doi:10.1002/ehf2.14405
PubMed | Crossref | Google Scholar - Teo SH, Chew EAL, Ng DWL, Tang WE, Koh GCH, Teo VHY. Implementation and use of technology-enabled blood pressure monitoring and teleconsultation in Singapore’s primary care: a qualitative evaluation using the socio-technical systems approach. BMC Prim Care. 2023;24(1):71. doi:10.1186/s12875-023-02014-8
PubMed | Crossref | Google Scholar - Jiang Y, Zheng L, Zhang Y, et al. Effectiveness of the intelligent hypertension excellence centers (iHEC) therapy model in the blood pressure management of older hypertensive patients: a randomized controlled trial. Hypertens Res. 2025;48(1):15-25. doi:10.1038/s41440-024-01951-w
PubMed | Crossref | Google Scholar
Acknowledgments
Not reported
Funding
No funding
Author Information
Corresponding Author:
Samatha Ampeti
Independent Researcher, Department of Content
medtigo India Pvt Ltd, Pune, India
Email: ampetisamatha9@gmail.com
Co-Authors:
Shubham Ravindra Sali, Mansi Srivastava, Raziya Begum Sheikh, Patel Nirali Kirankumar
Independent Researcher, Department of Content
medtigo India Pvt Ltd, Pune, India
Authors Contributions
All authors contributed to the conceptualization, investigation, and data curation by acquiring and critically reviewing the selected articles. They were collectively involved in the writing, original draft preparation, and writing – review & editing to refine the manuscript. Additionally, all authors participated in the supervision of the work, ensuring accuracy and completeness. The final manuscript was approved by all named authors for submission to the journal.
Ethical Approval
Not applicable
Conflict of Interest Statement
None
Guarantor
None
DOI
Cite this Article
Shubham RS, Samatha A, Mansi S, Raziya BS, Patel NK. Telemedicine in Chronic Cardiopulmonary and Cardiovascular Diseases: A Comprehensive Review. medtigo J Emerg Med. 2025;2(3):e30922310. doi:10.63096/medtigo30922310 Crossref




